
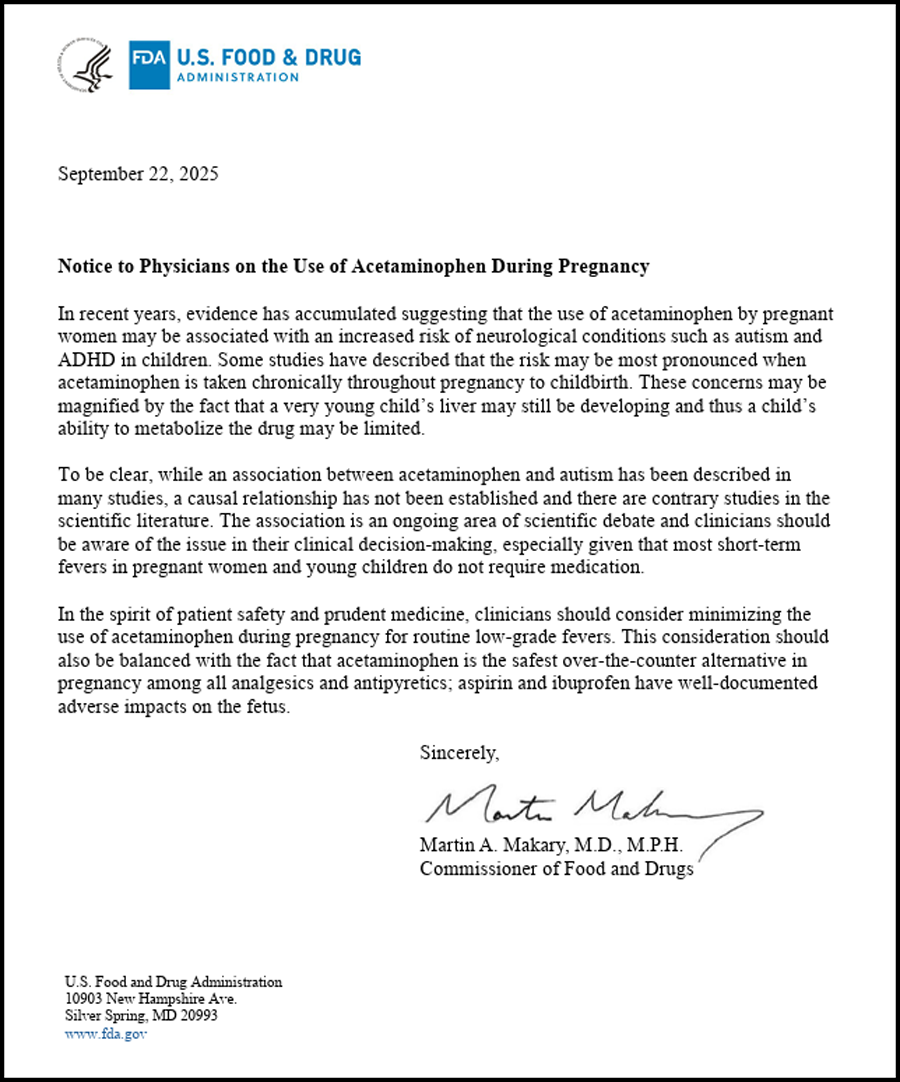
WASHINGTON, D.C. – The U.S. Food and Drug Administration has begun the formal process to update acetaminophen labeling with language indicating a possible association between use during pregnancy and later diagnoses of autism or ADHD in children. Alongside the move, the agency circulated a physician notice summarizing observational evidence and reiterating that a causal relationship has not been established. The FDA framed the step as a precaution in light of multiple large cohorts that report elevated odds of neurodevelopmental diagnoses among children with measured or reported prenatal exposure, particularly with chronic or frequent use.
Evidence remains mixed. A 2025 Environmental Health review using the Navigation Guide approach found that most included studies report positive associations with ADHD, ASD, or broader neurodevelopmental outcomes, while acknowledging substantial heterogeneity and residual confounding. Other analyses – some large registry studies – do not confirm a link. Specialists continue to warn that the reason for taking acetaminophen (e.g., maternal fever or infection) may drive part of the observed risk signal.
Obstetrics groups responded quickly. ACOG and SMFM both advised that acetaminophen remains an appropriate first-line option for pregnant patients when clinically indicated, especially to treat fever, which carries its own fetal risks. They characterize the current evidence as inconclusive and recommend individualized, lowest-effective-dose use.
Internationally, regulators are not aligned. The European Medicines Agency on Sept. 23 stated that the existing guidance stands, citing no new data warranting a change and advising continued use when necessary at the lowest effective dose.
The FDA action arrives amid elevated political attention and public debate. Major outlets and scientific journals stressed that association is not causation, even as policymakers highlighted specific studies. Clinics now anticipate increased patient questions; in practice, counseling is likely to emphasize balancing symptom control (especially fever) with prudent dosing and avoiding routine, prolonged use absent clinical need.
On the legal front, consumer lawsuits alleging failure-to-warn were set back when a federal judge dismissed the consolidated MDL in 2024 after excluding plaintiffs’ experts under Daubert; a Second Circuit appeal remains pending. Any FDA label change could influence future filings, but there is no settlement or liability finding at the federal level as of this week.
Quick Facts
| Category | Details |
|---|---|
| What Changed | FDA began a label update process for acetaminophen to reflect a possible association with autism/ADHD when used in pregnancy; also issued a physician notice. |
| Evidence Picture | Multiple observational studies report associations; other large studies do not; causation not established and confounding remains a concern. |
| OB Guidance Now | ACOG & SMFM say acetaminophen is still appropriate when clinically indicated; recommend lowest effective dose and avoiding prolonged, routine use. |
| International Stance | EMA keeps guidance unchanged: paracetamol remains acceptable in pregnancy when needed, lowest effective dose, shortest duration. |
| Known Alternatives | NSAIDs carry documented fetal risks in later pregnancy; untreated fever itself also poses risks to the fetus. |
| Lawsuits | Federal Tylenol–autism MDL dismissed in 2024 after expert exclusion; appeal pending before the Second Circuit, no ruling yet. |
Q&A
Q: Does the FDA say Tylenol causes autism?
A: No. The agency cites a possible association from observational studies and is moving to add precautionary wording, while noting causation is not established.
Q: Should pregnant patients stop using acetaminophen altogether?
A: Current medical guidance from ACOG/SMFM is no – use remains acceptable when clinically indicated, at the lowest effective dose, and avoid chronic, routine use without need. Always discuss with your clinician.
Q: What could actually change on store shelves?
A: If finalized, OTC labels may gain precautionary language about pregnancy use and potential neurodevelopmental risks, prompting more clinical counseling at point of care. (Label text and timing will go through FDA’s standard process.)
Q: How big is the potential risk?
A: Estimates vary by study design and exposure definition; some cohorts report modest increases in relative risk/odds, while others show no association after adjustment. There’s no agreed-upon causal risk estimate.
Q: What about Europe?
A: EMA reaffirmed no change to guidance; use when needed, lowest effective dose, shortest duration.
Q: Where do the lawsuits stand?
A: The federal MDL was dismissed after expert exclusion; appeal pending with no decision yet.
Sources To Support Key Claims
- FDA press announcement and newsroom index (label-change process; date; scope).
- FDA Notice to Physicians PDF (evidence summary; chronic use note).
- Environmental Health 2025 methodology review; representative cohort literature.
- ACOG FAQ/statement; SMFM statement (current clinical stance).
- EMA stance (Reuters same-day coverage).
- MDL status/appeal (recent legal summaries).


